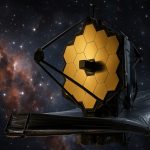
Revolutionizing Astronomy with Advanced Space Telescopes and Deep Space Observation
Eyes on the Infinite: How Next-Gen Space Telescopes Are Transforming Our Understanding of the UniverseExpanding Horizons: The Evolving Market for Space TelescopesCutting-Edge Innovations Shaping Space ObservationKey Players and Strategic Moves…
In-Depth Analysis of Warsaw’s Evolving Real Estate Sector
Unlocking the Future of Warsaw Real Estate: Trends, Insights, and Strategic PerspectivesMarket Overview: Key Drivers and Current DynamicsTechnology Trends Shaping Property Transactions and DevelopmentCompetitive Landscape: Major Players and Market ShareGrowth…
Quantum Gyroscopic Navigation Systems Market 2025: Surging Demand Drives 18% CAGR Through 2030
Quantum Gyroscopic Navigation Systems Market Report 2025: In-Depth Analysis of Growth Drivers, Technology Innovations, and Global Forecasts. Explore Key Trends, Competitive Dynamics, and Strategic Opportunities Shaping the Industry. Executive Summary…
Medical Stethoscopes Surge: Tech-Fueled Market Set to Skyrocket by 2032
Medical stethoscopes evolve with AI and Bluetooth, pushing the market toward $1.08B by 2032. See what’s driving this tech-fueled boom.
Hims & Hers Health Stock Skyrockets in 2025 — But Is This Telemedicine Sensation About to Crash?
Hims & Hers Health stock soared 157% in 12 months, outpacing AI giants — but experts see risk. Should investors cash in or stay away?
Medcorp Ltd Unveils Game-Changing IPO and Expansion Plans to Revolutionize Caribbean Healthcare
Medcorp Ltd launches its IPO, eyeing satellite campuses and digital innovation to transform healthcare access across the Caribbean.
Medicare’s Telehealth Shake-Up: DOJ’s Latest Fraud Conviction Puts 2025 Coverage Under Fire
The Justice Department’s latest conviction rocks Medicare’s telehealth program, fueling urgent reform talks and 2025 policy debates.
Veterinary Telemedicine Booms: Why 2025 Will Be a Breakout Year for Pet Healthcare Tech
Inside the Rapid Rise of Veterinary Telemedicine: How Digital Health Is Changing Pet Care in 2025 and Beyond The veterinary telemedicine market is set for explosive growth. Find out why…
Arkansas Loses $10.7M Telemedicine Grant as Federal Digital Equity Program Gets Axed
Digital Equity Dreams Shattered: UAMS Left in Limbo as $10.7 Million Broadband Grant Pulled Amid Program Shutdown UAMS and partners left scrambling as a multi-million dollar federal grant for Arkansas…
AI, IoT, and Telemedicine Are Rewiring Global Healthcare: Here’s What’s Coming in 2025
The Future of Health: Game-Changing Tech Set to Revolutionize Care in 2025 and Beyond Discover how AI, IoT, telemedicine, and smart devices will deliver faster, smarter, and more accessible healthcare…